COVID-19 vaccine rollouts are last but not least upon us. They hope that herd immunity—protection from an infectious ailment that takes place after a adequate proportion of the populace has been vaccinated or infected—is on the horizon. But even while the first vaccines to get emergency use authorization from the U.S. Foodstuff and Drug Administration are extremely effective at preventing COVID-19, facts are unable to nonetheless convey to us if they hinder transmission of SARS-CoV-2, the virus that results in the disease.
The concern of whether or not immunization helps prevent recipients from getting to be sick and from infecting other people is not exclusive to the existing pandemic. In accordance to Dawn Bowdish, a professor of pathology and molecular medication at McMaster College, this so-referred to as sterilizing immunity was a critical variable in eradicating smallpox.
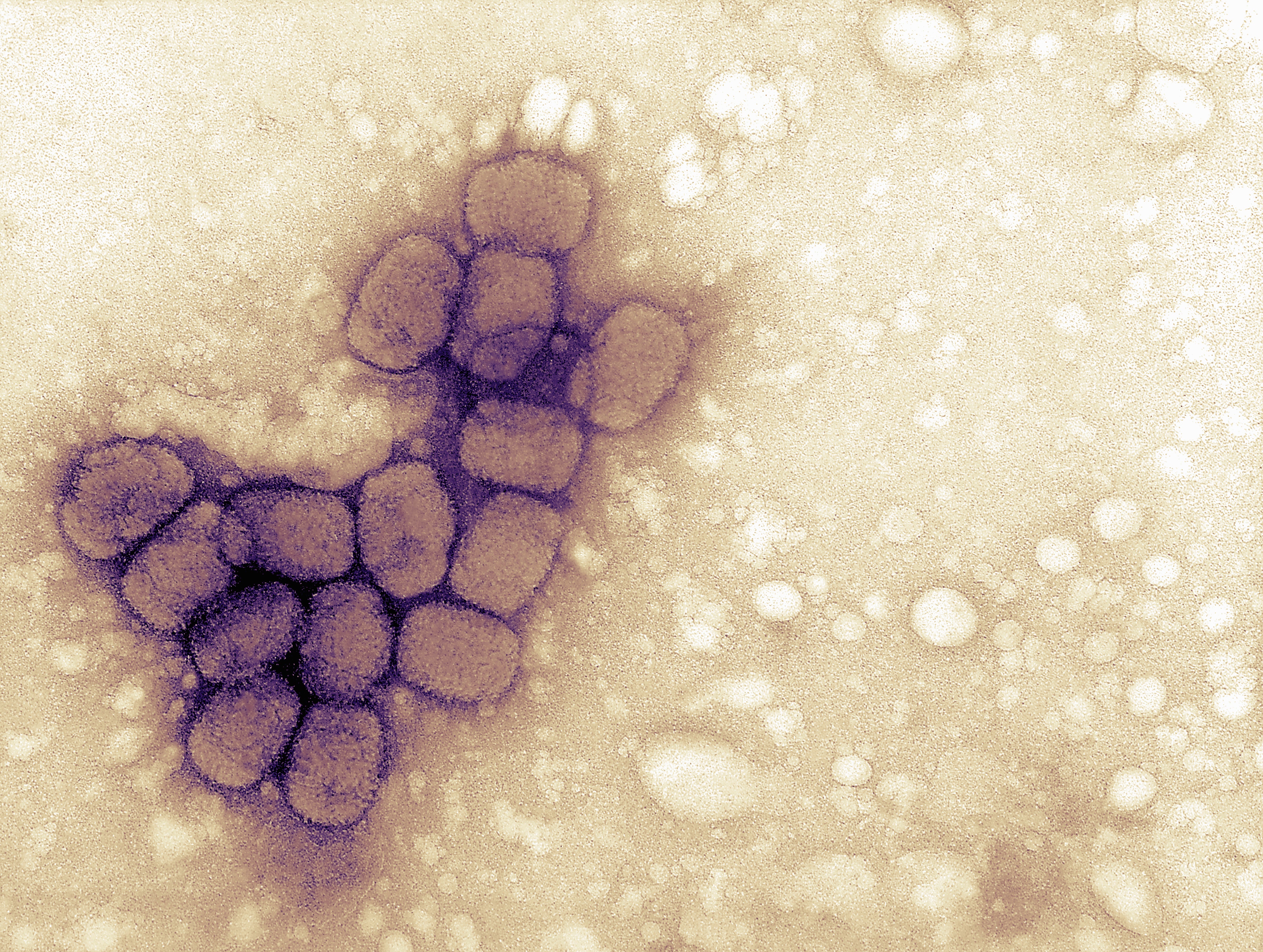
The smallpox, or variola, virus ravaged human populations for countless numbers of many years, evidenced by traces of pustules located on the 3,000-year-aged mummy of Egyptian pharaoh Ramses V. Stories show the virus was spreading globally by the initial century C.E., and it at some point turned a hundreds of years-extensive pandemic. Historians consider the condition killed far more than 300 million people concerning 1900 and its formal eradication in 1980. “Smallpox transformed the record of the world—changing royal successions and the results of wars that afflicted the destinies of total international locations,” states Natasha Crowcroft, senior specialized adviser for measles and rubella at the World Wellness Corporation.
The combat towards smallpox inspired early inoculation endeavours and led to English doctor Edward Jenner’s cowpox vaccine versus smallpox in 1796. “The [smallpox] vaccination brought on sterilizing immunity, indicating that you never carry any of the virus. The antibodies that you deliver, the responses you generate, clear the virus from your technique completely,” Bowdish claims.
While numerous vaccines greatly made use of right now (in opposition to measles, for example) make incredibly productive sterilizing immunity, other individuals, these as the hepatitis B vaccine, do not. With these vaccines, an individual’s immune system is properly trained to stop ailment, but the pathogen can persist in that person’s physique, perhaps letting them to infect other individuals. A absence of sterilizing immunity means that the pathogen can proceed to flow into in a population, wherever it may possibly cause disease in unvaccinated and susceptible persons or evolve to evade our immune responses, Bowdish points out.
Sterilizing immunity could have been a lofty aim for COVID-19 vaccine makers, nevertheless not needed to suppress sickness. In accordance to Crowcroft, the pretty notion of this kind of immunity is nuanced. “In fact, the spectrum of security may greatest be framed as the extent to which vaccination prevents transmission of the wild-style virus or bacteria,” she says.
The scenario of rotavirus—which leads to severe vomiting and watery diarrhea and is in particular risky to infants and younger children—is relatively clear-cut. Vaccination boundaries, but does not end, the pathogen from replicating. As these types of, it does not protect in opposition to gentle ailment. By reducing an infected person’s viral load, on the other hand, it decreases transmission, providing considerable indirect security. According to the Facilities for Condition Handle, 4 to 10 many years following the 2006 introduction of a rotavirus vaccine in the U.S., the variety of constructive checks for the illness fell by as substantially as 74 to 90 percent .
The pathway to vaccine-mediated command of an infectious ailment is not constantly so immediate. Eventually, whether or not, and to what degree, inoculation helps prevent transmission depends on the pathogen itself, the host or hosts it infects and the conversation concerning the two, Bowdish claims.
For illustration, vaccines from Bordetella pertussis, the primary bacterium that will cause whooping cough, or pertussis, do a great work of avoiding sickness but do not completely crystal clear the pathogen. Alternatively, as B. pertussis replicates in the higher respiratory tract, vaccine-induced antibodies apply force via pure range to weed out micro organism whose sickness-leading to genes are turned on. Mainly because these identical genes are dependable for the elements of the microorganisms that are targeted by antibodies, germs that preserve them turned off evade the immune reaction and dangle out undetected in the higher respiratory tract, Bowdish clarifies. This turns into a dilemma when a person with a naive immune process, this kind of as an toddler, contracts the pathogen. In the absence of antibodies, B. pertussis’s disorder-causing genes become activated once more, creating illness. Nevertheless, the introduction of pertussis vaccines in the 1940s lower annual U.S. situations from far more than 100,000 to fewer than 10,000 by 1965. In the 1980s conditions commenced little by little climbing once again as parents significantly refused to vaccinate their youngsters. Currently there is renewed target on minimizing the possibility of publicity and receiving antibodies to infants by immunizing pregnant females and new mothers.
Endeavours to arrest the spread of polio give extra insight into the complexity of halting an epidemic. The two principal classes of inoculations in opposition to polioviruses confer different forms of immunity. The inactivated polio vaccine (IPV) guards from systemic an infection and consequent paralysis but does not quit viral replication in the gut, so it offers no oblique protection to unvaccinated folks. The oral polio vaccine (OPV) generates localized intestinal immunity, stopping infection and preserving towards sickness and transmission. For the reason that the OPV takes advantage of a weakened stay poliovirus, nonetheless, in unusual cases amongst underimmunized populations, the attenuated virus mutates, circulates and as soon as once more causes ailment. The International Polio Eradication Initiative and the Environment Wellbeing Firm advocate distinctive vaccination methods relying on the regional context. In locations exactly where wild polio even now exists, OPV is vital to slowing transmission. In locations the place the wild virus has been eradicated, IPV keeps populations protected. Many thanks to prevalent immunization courses, the U.S. has been polio-free considering that 1979, and the condition is on the verge of world wide eradication.
In a paper in the Oct 2020 concern of the American Journal of Preventive Medicine, scientists modeled what a COVID-19 vaccine with varying styles of protection could imply. They identified that if a vaccine safeguards 80 percent of those immunized and 75 {0841e0d75c8d746db04d650b1305ad3fcafc778b501ea82c6d7687ee4903b11a} of the populace is vaccinated, it could mostly close an epidemic without other measures these as social distancing. “Otherwise, you will not be capable to depend on the vaccine to return us to ‘normal,’” suggests Bruce Y. Lee, a co-creator of the paper and a professor at the CUNY Graduate School of Community Health and Health Coverage. That is, if the vaccine only helps prevent disease or lessens viral shedding somewhat than eliminating it, supplemental public overall health actions might nevertheless be needed. Even so, Lee stressed that a widespread nonsterilizing vaccine could still reduce burden on the health treatment program and help save lives.
Influenza may perhaps deliver the very best blueprint of what to expect going ahead. The most prevalent flu vaccine—the inactivated virus—is not “truly sterilizing due to the fact it does not create neighborhood immune reaction in the respiratory tract,” Crowcroft claims. This truth, coupled with minimal immunization costs (frequently shy of 50 p.c amongst grownups) and the influenza virus’s ability to infect and go involving many species, allows it to continuously alter in ways that make it tough for our immune technique to acknowledge. Even now, based on the year, flu vaccines have been demonstrated to cut down hospitalizations between more mature adults by an believed 40 per cent and intensive treatment admissions of all grownups by as significantly as 82 per cent.
Exploration on seasonal coronaviruses implies that SARS-CoV-2 could in the same way evolve to evade our immune programs and vaccination attempts, though probably at a slower tempo. And facts continue to be blended on the romance concerning signs and symptoms, viral load and infectiousness. But sufficient precedent details to vaccines driving successful containment of infectious health conditions even when they do not give properly sterilizing immunity. “Measles, diphtheria, pertussis, polio, hepatitis B—these are all epidemic-inclined diseases,” Crowcroft states. “They show that we never need 100 per cent success at lowering transmission, or 100 percent coverage or 100 {0841e0d75c8d746db04d650b1305ad3fcafc778b501ea82c6d7687ee4903b11a} usefulness towards sickness to triumph in excess of infectious ailments.”
Browse much more about the coronavirus outbreak from Scientific American below. And go through coverage from our intercontinental community of journals listed here.